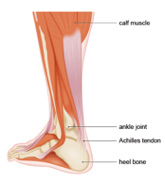
 The “Achilles Tendon” is the largest and strongest tendon (a tough band of fibrous tissue) in the body where the calf muscles unite into one band of tissue. It is found at the back of the leg right above the heel and connects the calf muscles at the back of the lower leg to the heel bone. The “Achilles Tendon” pulls on the heel when the calf muscles flex allowing several movements such as standing on the toes, walking, running and jumping.
The “Achilles Tendon” is the largest and strongest tendon (a tough band of fibrous tissue) in the body where the calf muscles unite into one band of tissue. It is found at the back of the leg right above the heel and connects the calf muscles at the back of the lower leg to the heel bone. The “Achilles Tendon” pulls on the heel when the calf muscles flex allowing several movements such as standing on the toes, walking, running and jumping.
Due to the high tension that the Achilles tendon is subjected to and the fact that it has a limited blood supply, injuries can occur to it causing pain. Pain around the “Achilles Tendon” is mainly caused by tendon overuse, repeated movements or injuries during daily activities or sports. The pain may appear suddenly but it’s mostly a result of accumulated minor tendon injuries or tears that have happened over time but the patient was unaware of them.
Around the Achilles tendon pain could be mild or severe and is usually associated with ankle swelling. The pain could be constant or felt only when the patient attempts to walk or run. There could also be a weakness in the movement of the ankle. When the tendon is injured there is usually a sudden sharp pain often accompanied by a popping sound indicating that the tendon has been ruptured.
Swelling and bruising may also occur to the extent that the patient can’t put his/her foot down or stand up. Depending on the cause and extent of pain, sometimes home rest and the use of painkillers can help reduce the pain but if the pain persists medical intervention is required.
1. Achilles Tendiopathy (Tendinitis/Tendinosis):
Is a common condition that causes pain, swelling, stiffness and weakness around the Achilles tendon and is usually caused by the overuse and/or repeated injuries of the tendon. This is a general term used to describe:
– Tendinitis: the inflammation of the tendon caused by frequent activity which causes pain and stiffness at the back of the heel.
– Tendinosis: the thickening of the tendon that happens gradually without visible inflammation usually due to aging and/or tendon overuse.
2. Achilles Tendon Tear/Rupture:
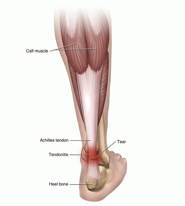 The tendon could be torn in small microtears or larger tears that usually cause pain and swelling as well as inhibit the patient’s movement. The tears could occur gradually over time or suddenly due to a sports injury or a wrong move.
The tendon could be torn in small microtears or larger tears that usually cause pain and swelling as well as inhibit the patient’s movement. The tears could occur gradually over time or suddenly due to a sports injury or a wrong move.
Achilles tendon complete rupture could happen usually causing a popping sound at the time of the rupture. After the tendon is ruptured there is often severe pain and swelling of the lower part of the injured leg.
3. Achilles or heel Bursitis:
The “Bursa” is a small, fluid-filled sac that cushions the Achilles tendon at the heel area to reduce friction between the bones and the overlying soft tissues.
Overuse of the ankle can irritate the bursa and inflame it. This usually happens with repeated walking, running or jumping. The skin at the back of the heel may become red and warm due to the irritation. Pain may be felt in the heel especially while walking, running or even touching the area. Achilles Bursitis pain gets even worse when the patient attempts to stand on his/her toes.
1. Medication:
– Using anti inflammatory medications which provides varying results from one patient to the other and typically gives short term relief and is ineffective with others.
2. Physiotherapy:
– Performing some physiotherapy exercises with a specialist. This may provide a relief of pain after many sessions. This could be ineffective and some patients do not prefer this type of long course treatment.
3. Pain Killers and Exercise:
– This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months.
4. Surgical Intervention:
– Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anesthesia.
5. Localized pain management injection without image guidance:
– This technique relies on injecting certain medication to the pain area at a doctor’s clinic (not radiologist) to relieve the pain. This approach may result in many complications due to the fact that the doctor can’t see where he injected the medication, so he may inject the wrong spot without any benefit and sometimes even causes even more pain and discomfort to the patient. Statistic accurate localization of painful spot is about 10-30%.
6. Localized pain management injection with ultrasound guidance (our preferred method of administrating the medication):
– This is a modern, advanced, non surgical treatment technique that relies on injecting specific medication accurately into the area of inflammation under ultrasound guidance. Using an accurate, effective, safe and non invasive technique, make us achieve better results in terms of pain relief/management. Statistic accuracy rate is about 95-99%.
This technique uses FDA approved medication, which is injected, directly into the pain area under ultrasound guidance. This technique has the following benefits:
– Helps the radiologist to accurately identify the inflamed tendon or bursa, which is important to confirm the clinical examination.
– Allows the radiologist to accurately localize and effectively administer the medicine to one or more compartments of the painful area “if necessary” resulting in better and faster pain relief.
– The patient benefits the most by having the medication in the right spot without pain or complications.
– The patient is injected a numbing local anesthetic. A mild burning sensation can be felt due to the numbing anesthetic.
– The radiologist then uses an ultrasound probe to guide the needle to the painful area.
– The medication is then injected in the exact location.
– The injection needle is then removed.
– The patient can leave immediately after the injection. Some patients may be asked to wait for re assessment.
– After the procedure the patient may experience complete relief of pain.
– The maximum effect of the medications may take up to 2 weeks to show the maximum effect.
– The patient is instructed to use painkillers during the first few days if needed.
Different patients respond differently to the same. So one may have a total relief and others may have residual pain and would benefit from another injection.
Most patients report the following after the procedure:
– A great reduction or total elimination of the pain for a period of several weeks after which they may need to have another injection to maintain the results.
– A great reduction or elimination of the pain for several months.
– A great reduction or elimination of pain for years after the procedure especially if complimented with physiotherapy.
Other Treatments

Medication
Using oral or intra muscular anti-inflammatory medications provides varying results from one patient to other, typically giving short-term relief. This may be ineffective with some patients.

Physiotherapy
Performing some physiotherapy exercises with a specialist may relief shoulder pain after many sessions. This may be in effective and difficult with some patient due to the severe shoulder pain, which means that the patient may not be able to perform the recommended exercises.

Pain Killers & Exercise
This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months or longer..

Surgical Intervention
Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anaesthesia.

Comments
Currently have