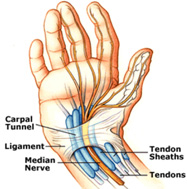
 The “Carpal Tunnel” is a thin canal found on the palmar side of the wrist and connects the forearm to the middle section of the palm. This passageway acts as house through which the “Median Nerve”, tendons and certain muscles of the hands pass through. The Median Nerve is a nerve in the upper limb that runs through the forearm to the palm of the hand connecting the thumb and all fingers except for the little finger.
The “Carpal Tunnel” is a thin canal found on the palmar side of the wrist and connects the forearm to the middle section of the palm. This passageway acts as house through which the “Median Nerve”, tendons and certain muscles of the hands pass through. The Median Nerve is a nerve in the upper limb that runs through the forearm to the palm of the hand connecting the thumb and all fingers except for the little finger.
Carpal Tunnel Syndrome is the pressing or squeezing of the median nerve at the wrist. The median nerve is mainly responsible for delivering the sensations to the palm side of the thumb and fingers (excluding the little finger), as well as the movement of the fingers, thumb and hand.
When the Carpal Tunnel becomes narrowed it compresses the Median Nerve, causing a painful, progressive condition called “Carpal Tunnel Syndrome”. Sometimes the Median Nerve becomes compressed due to irritation or swelling of the tendons, which in turn narrows the Carpal Tunnel.
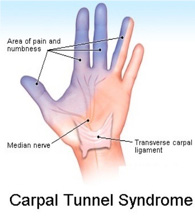 The pain may be manifested in the form of weakness, numbness and/or tingling on the palm side of the thumb, index, middle, and ring fingers. It may also radiate to the forearm or shoulder and the hand may become numb. Some patients lose the ability to feel different hot and cold temperatures.
The pain may be manifested in the form of weakness, numbness and/or tingling on the palm side of the thumb, index, middle, and ring fingers. It may also radiate to the forearm or shoulder and the hand may become numb. Some patients lose the ability to feel different hot and cold temperatures.
Sometimes the pain in the hand and wrist weaken the strength of the patient’s grip and he/she may drop things. Commonly both hands are inflicted even if only one hand has obvious symptoms, the other if tested will show that it too is inflicted.
The patient may experience swelling or feel that his/her hands are swollen even if the swelling is not visible. Symptoms may occur at rest and may even wake the patient up during sleep.
At the early stages of Carpal Tunnel Syndrome, resting every now and then and not stressing the hand usually relieves the numbness and pain. The patient may also use non steroidal anti inflammatory drugs to ease the pain and use ice packs on the wrist as needed. Some patients also wear a wrist support splint especially while sleeping to support the wrist’s position. However, when the pain persists at later stages of the syndrome, medical intervention is required.
Carpal Tunnel Syndrome is considered an inflammatory disorder that may result from repeated stress, a medical condition or physical injury. There is no clear cut procedure or test whereby the exact cause of Carpal Tunnel Syndrome may be determined.
Whereas previous studies have indicated that above 50% of the cases result from working conditions; nowadays, research shows that the syndrome is directly related to certain health conditions such as diabetes, osteoarthritis, hypothyroidism and rheumatoid arthritis.
1. Medication:
– Using anti inflammatory medications which provides varying results from one patient to the other and typically gives short term relief and is ineffective with others.
2. Physiotherapy:
– Performing some physiotherapy exercises with a specialist. This may provide a relief of pain after many sessions. This could be ineffective and some patients do not prefer this type of long course treatment.
3. Pain Killers and Exercise:
This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months.
4. Surgical Intervention:
Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anesthesia.
5. Localized pain management injection without image guidance:
This technique relies on injecting certain medication to the pain area at a doctor’s clinic (not radiologist) to relieve the pain. This approach may result in many complications due to the fact that the doctor can’t see where he injected the medication, so he may inject the wrong spot without any benefit and sometimes even causes even more pain and discomfort to the patient. Statistic accurate localization of painful spot is about 10-30%.
6. Localized pain management injection with ultrasound guidance (our preferred method of administrating the medication):
This is a modern, advanced, non surgical treatment technique that relies on injecting specific medication accurately into the area of inflammation under ultrasound guidance. Using an accurate, effective, safe and non invasive technique, make us achieve better results in terms of pain relief/management. Statistic accuracy rate is about 95-99%.
This technique uses FDA approved medication, which is injected, directly into the pain area under ultrasound guidance. This technique has the following benefits:
– Helps the radiologist to accurately identify the inflamed tendon or bursa, which is important to confirm the clinical examination.
– Allows the radiologist to accurately localize and effectively administer the medicine to one or more compartments of the painful area “if necessary” resulting in better and faster pain relief.
– The patient benefits the most by having the medication in the right spot without pain or complications.
– The patient is injected a numbing local anesthetic. A mild burning sensation can be felt due to the numbing anesthetic.
– The radiologist then uses an ultrasound probe to guide the needle to the painful area.
– The medication is then injected in the exact location.
– The injection needle is then removed.
– The patient can leave immediately after the injection. Some patients may be asked to wait for re assessment.
– After the procedure the patient may experience complete relief of pain.
– The maximum effect of the medications may take up to 2 weeks to show the maximum effect.
– The patient is instructed to use painkillers during the first few days if needed.
Different patients respond differently to the same. So one may have a total relief and others may have residual pain and would benefit from another injection.
Most patients report the following after the procedure:
– A great reduction or total elimination of the pain for a period of several weeks after which they may need to have another injection to maintain the results.
– A great reduction or elimination of the pain for several months.
– A great reduction or elimination of pain for years after the procedure especially if complimented with physiotherapy.
Other Treatments

Medication
Using oral or intra muscular anti-inflammatory medications provides varying results from one patient to other, typically giving short-term relief. This may be ineffective with some patients.

Physiotherapy
Performing some physiotherapy exercises with a specialist may relief shoulder pain after many sessions. This may be in effective and difficult with some patient due to the severe shoulder pain, which means that the patient may not be able to perform the recommended exercises.

Pain Killers & Exercise
This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months or longer..

Surgical Intervention
Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anaesthesia.

Comments
Currently have