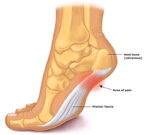
 The “Plantar Fascia” is a thick fibrous band of connective tissue (ligament) found at the sole (bottom) of the foot and connects the heel bone to the toes. This connective tissue is attached to the heel bone called the (calcaneus) and divides and spans out to attach at the base of the toes, where the bone between each toe and the bones of the mid foot are.
The “Plantar Fascia” is a thick fibrous band of connective tissue (ligament) found at the sole (bottom) of the foot and connects the heel bone to the toes. This connective tissue is attached to the heel bone called the (calcaneus) and divides and spans out to attach at the base of the toes, where the bone between each toe and the bones of the mid foot are.
The plantar fascia functions as a cover for layers of muscles, tendons, nerves, and blood vessels found at the bottom of the foot where it covers these layers and helps the bones of the foot maintain their arch. A fat pad is found covering the plantar fascia right beneath the heel bone. This pad acts as a cushion to the heel as it absorbs the shock of every footstep.
Pain in the plantar fascia is known as “Plantar Fasciitis”, a term used to cover the condition that involves pain and inflammation of the plantar fascia. Symptoms include stabbing pain that usually happens with the first morning steps at the underside of the heel. The pain diminishes with movement, however, long stands or standing up after being seated for a while may trigger an intense pain. The pain may also arise with climbing stairs.
Plantar Fasciitis is a very common condition that could cause a lot of pain if not attended to in the right way. Certain conditions make people susceptible to plantar fascia, these include increased activities as with runners and especially when running on hard surfaces, being overweight, old age and those who wear shoes that do not provide ample foot support. Depending on the cause and extent of pain, sometimes home rest and the use of painkillers can help reduce the pain but if the pain persists medical intervention is required.
Medicine has not arrived at a decisive conclusion regarding the causes of plantar fasciitis or plantar fascia pain. However, it is thought to be a result of repeated small tears, stress or strain due to the way the patient walks along with other conditions; these include:
1. Abnormal Inward Twisting of the Foot (Excessive Pronation):
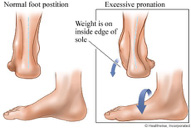 This is a condition where the weight of the patient’s body stays on the inner edge of the foot sole as opposed to the normal pronation where the foot lands on the outer side of the feet first during walking. Excessive pronation is seen when the patient is standing up, the foot appears rolled inward which accordingly makes the foot arch flatten causing plantar fasciitis.
This is a condition where the weight of the patient’s body stays on the inner edge of the foot sole as opposed to the normal pronation where the foot lands on the outer side of the feet first during walking. Excessive pronation is seen when the patient is standing up, the foot appears rolled inward which accordingly makes the foot arch flatten causing plantar fasciitis.
2. Repetitive Activities:
Certain repetitive activities may also cause plantar fasciitis. These activities could be sports related such as running, or work related such as long standing times or walking on irregular ground surfaces.
3. Obesity or Being Overweight:
Being overweight adds extra stress to the feet and may in time particularly if the patient wears uncomfortable shoes or shoes that don’t properly support the foot lead to plantar fascia pain.
4. Aging:
Plantar Fasciitis is most commonly seen with patients of middle age and older. The natural aging process with the wear and tear of the plantar fascia may in time cause plantar fasciitis.
5. Heel Spurs:
Heel spurs are often connected with plantar fasciitis. A heel spur is generally caused by the deposit of calcium at the bottom of the heel bone. The protrusion of a heel spur can stretch forward by approximately half-inch and is detected by an X-ray.
1. Medication:
– Using anti inflammatory medications which provides varying results from one patient to the other and typically gives short term relief and is ineffective with others.
2. Physiotherapy:
– Performing some physiotherapy exercises with a specialist. This may provide a relief of pain after many sessions. This could be ineffective and some patients do not prefer this type of long course treatment.
3. Pain Killers and Exercise:
This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months.
4. Surgical Intervention:
Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anesthesia.
5. Localized pain management injection without image guidance:
This technique relies on injecting certain medication to the pain area at a doctor’s clinic (not radiologist) to relieve the pain. This approach may result in many complications due to the fact that the doctor can’t see where he injected the medication, so he may inject the wrong spot without any benefit and sometimes even causes even more pain and discomfort to the patient. Statistic accurate localization of painful spot is about 10-30%.
6. Localized pain management injection with ultrasound guidance (our preferred method of administrating the medication):
This is a modern, advanced, non surgical treatment technique that relies on injecting specific medication accurately into the area of inflammation under ultrasound guidance. Using an accurate, effective, safe and non invasive technique, make us achieve better results in terms of pain relief/management. Statistic accuracy rate is about 95-99%.
This technique uses FDA approved medication, which is injected, directly into the pain area under ultrasound guidance. This technique has the following benefits:
– Helps the radiologist to accurately identify the inflamed tendon or bursa, which is important to confirm the clinical examination.
– Allows the radiologist to accurately localize and effectively administer the medicine to one or more compartments of the painful area “if necessary” resulting in better and faster pain relief.
– The patient benefits the most by having the medication in the right spot without pain or complications.
– The patient is injected a numbing local anesthetic. A mild burning sensation can be felt due to the numbing anesthetic.
– The radiologist then uses an ultrasound probe to guide the needle to the painful area.
– The medication is then injected in the exact location.
– The injection needle is then removed.
– The patient can leave immediately after the injection. Some patients may be asked to wait for re assessment.
– After the procedure the patient may experience complete relief of pain.
– The maximum effect of the medications may take up to 2 weeks to show the maximum effect.
– The patient is instructed to use painkillers during the first few days if needed.
Different patients respond differently to the same. So one may have a total relief and others may have residual pain and would benefit from another injection.
Most patients report the following after the procedure:
– A great reduction or total elimination of the pain for a period of several weeks after which they may need to have another injection to maintain the results.
– A great reduction or elimination of the pain for several months.
– A great reduction or elimination of pain for years after the procedure especially if complimented with physiotherapy.
Other Treatments

Medication
Using oral or intra muscular anti-inflammatory medications provides varying results from one patient to other, typically giving short-term relief. This may be ineffective with some patients.

Physiotherapy
Performing some physiotherapy exercises with a specialist may relief shoulder pain after many sessions. This may be in effective and difficult with some patient due to the severe shoulder pain, which means that the patient may not be able to perform the recommended exercises.

Pain Killers & Exercise
This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months or longer..

Surgical Intervention
Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anaesthesia.

Comments
Currently have