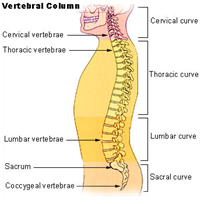
The back is the part of the body that starts from the bottom back of the neck to the top of the buttocks. The “Vertebral Column” often called “Spine” or “back bone” runs through the back from top to bottom and comprises the length of the back.
The vertebral column is composed of several vertebrae that receive motor and sensory signals by the spinal nerve.
Back pain is pain felt in any part of the “vertebral column” or “spine”. It can be temporary or chronic and can also be constant or sporadic. The pain can be in the form of an aching or a burning sensation, inflammation or a sharp piercing pain that could even radiate to the shoulder, arms or legs according to the cause of the pain.
Back pain originates in one or more of the structures of the “vertebral column” or “spine”:
- Cervical: the 7 top vertebrae in the neck region immediately beneath the
 scull.
scull. - Thoracic: the 12 vertebrae of the middle section of the spine to which the ribcage is attached.
- Lumbar: the 5 vertebrae of the lower back between the end of the ribcage and the pelvis.
- Sacral: the 5 bottom vertebrae that form the “sacrum” (the triangular bone between the hipbones of the pelvis).
Back pain occurs due to several reasons; these include:
1.Back Strain:
This condition occurs when the series of muscles and ligaments in the back holding the “spine” or “vertebral column” in place become weakened and accordingly start causing pain.
– Most back strain occurs in the lower back where the back is least supported in the region right after the ribcage. The strain can be caused by over stretching the back muscles which creates some tears in the muscle tissue or through heavy exercising, falling or lifting heavy things.
-It can also be caused by being overweight, being out of shape due to lack of exercise, sitting in the same position for long times or even sitting in the wrong posture.
2.Sciatic Pain:
Sciatic pain is a very common type of pain felt in the lower back behind the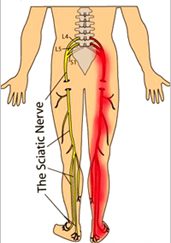 thigh and usually radiates to the back of the knee and is felt on one side of the body. It’s generally caused by the compression, irritation or inflammation of the “Sciatic Nerve” which extends from the lower end of the back and runs through the buttocks and divides above the knees.
thigh and usually radiates to the back of the knee and is felt on one side of the body. It’s generally caused by the compression, irritation or inflammation of the “Sciatic Nerve” which extends from the lower end of the back and runs through the buttocks and divides above the knees.
-The main cause for Sciatica is lumbar disk herniation (a tear in the outer layer of one of the lumbar intervertebral disks that causes the soft central material of the disk to bulge out). The disk herniation directly compresses the “Sciatic nerve” causing Sciatic pain.
-An irritation or inflammation to the nerve sometimes even caused by an adjacent bone or muscle can also cause Sciatic pain. Sometimes the Sciatic nerve can also become irritated during pregnancy.
3.Herniated Disc:
A disc is a rounded pad of dense fibrous tissue that forms a joint between two adjacent vertebrae to allow their movement and hold them together. Disc herniation is defined as the bulging out of the soft central material of an intervertebral disc due to a tear in its outer layer.
-The most common cause of disc herniation is aging. As individuals age, the discs lose some of the fluid inside of them that allows them to remain flexible. This is known as the wear and tear of discs and is often referred to as “Disc Degeneration”. Other causes for disc herniation include sports injuries, a sudden strain or twist to the lower back or a sudden or improper lifting of a heavy object.
-Depending on whether the herniated disc is compressing a nerve or not, the pain associated with it can range from mild ache to severe pain, numbness and/or weakness in the area to which the nerve travels. Also, the location of the herniated disc determines the part of the back where the pain will be and the other parts of the body to which it can radiate.
4.Back/Spinal Arthritis:
Arthritis (a painful inflammation and stiffness of the joints) is a very common problem that affects the lumbar spine. It is commonly found in elderly but can also be seen at any age. After the age of 45, it is most commonly seen in females more than males.
-Osteoarthritis of the spine (a degeneration of the joint cartilage and discs of the neck and lower back) is the most common type of spinal arthritis and is often referred to as “Spondylosis”. This condition causes lower back pain and stiffness in the back movements.
-Spinal arthritis is most commonly seen in patients who are overweight. Individuals who have jobs that involve stressing certain joints of the back are more susceptible to developing arthritis of the spine.
5.Spinal Stenosis:
The spinal cord is a bundle of nerves and fibers that are housed inside a canal in the “spine” or “vertebral column” and from which the spinal nerves branch out and extend to the rest of the body. When the space or canal surrounding the spinal cord becomes narrowed, this condition is known as “Spinal Stenosis”.
-With “Spinal Stenosis”, the spinal cord nerves or the nerves branching out from it become compressed causing pain, numbness, muscle weakness and/or tingling in either the arms or legs depending on the area of narrowing.
-Most common causes for “Spinal Stenosis” are degenerative age related conditions such as bone spurs growing into the spinal canal, spinal arthritis, thickened ligaments that cause them to bulge into the spinal canal. Spinal injuries or accidents may also dislocate a bone causing it to intervene with the spinal canal space causing nerve compression.
1. Medication:
-Using anti inflammatory medications which provides varying results from one patient to the other and typically gives short term relief and is ineffective with others.
2. Physiotherapy:
-Performing some physiotherapy exercises with a specialist. This may provide a relief of pain after many sessions. This could be ineffective and some patients do not prefer this type of long course treatment.
3. Pain Killers and Exercise:
-This approach relies on using painkillers combined with stretching exercises and waiting for the pain to improve. This may show an effect within 1 to 6 months.
4. Surgical Intervention:
-Some patients resort to surgery to end the severe pain. This approach has varying results according to the cause and severity of the pain and carries the common risks associated with any surgery or undergoing general anesthesia.
5. Localized pain management injection without image guidance:
-This technique relies on injecting certain medication to the pain area at a doctor’s clinic (not radiologist) to relieve the pain. This approach may result in many complications due to the fact that the doctor can’t see where he injected the medication, so he may inject the wrong spot without any benefit and sometimes even causes even more pain and discomfort to the patient. Statistic accurate localization of painful spot is about 10-30%.
6. Localized pain management injection with ultrasound guidance (our preferred method of administrating the medication):
-This is a modern, advanced, non surgical treatment technique that relies on injecting specific medication accurately into the area of inflammation under ultrasound guidance. Using an accurate, effective, safe and non invasive technique, make us achieve better results in terms of pain relief/management. Statistic accuracy rate is about 95-99%.
This technique uses FDA approved medication, which is injected, directly into the pain area under ultrasound guidance. This technique has the following benefits:
-Helps the radiologist to accurately identify the inflamed tendon or bursa, which is important to confirm the clinical examination.
-Allows the radiologist to accurately localize and effectively administer the medicine to one or more compartments of the painful area “if necessary” resulting in better and faster pain relief.
-The patient benefits the most by having the medication in the right spot without pain or complications.
-The patient is injected a numbing local anesthetic. A mild burning sensation can be felt due to the numbing anesthetic.
-The radiologist then uses an ultrasound probe to guide the needle to the painful area.
-The medication is then injected in the exact location.
-The injection needle is then removed.
-The patient can leave immediately after the injection. Some patients may be asked to wait for re assessment.
-After the procedure the patient may experience complete relief of pain.
-The maximum effect of the medications may take up to 2 weeks to show the maximum effect.
-The patient is instructed to use painkillers during the first few days if needed.
Different patients respond differently to the same. So one may have a total relief and others may have residual pain and would benefit from another injection.
Most patients report the following after the procedure:
-A great reduction or total elimination of the pain for a period of several weeks after which they may need to have another injection to maintain the results.
-A great reduction or elimination of the pain for several months.
-A great reduction or elimination of pain for years after the procedure especially if complimented with physiotherapy.

Comments
Currently have